Невротизация лицевого нерва как эффективный способ лечения паралича мимической мускулатуры
- Авторы: Скалийчук Б.В.1, Гайворонский А.И.1,2, Виноградов В.В.1, Свистов Д.В.1
-
Учреждения:
- Военно-медицинская академия им. С.М. Кирова
- Санкт-Петербургский государственный университет
- Выпуск: Том 104, № 1 (2023)
- Страницы: 134-143
- Раздел: Обмен клиническим опытом
- Статья получена: 24.12.2021
- Статья одобрена: 29.09.2022
- Статья опубликована: 01.02.2023
- URL: https://kazanmedjournal.ru/kazanmedj/article/view/90970
- DOI: https://doi.org/10.17816/KMJ90970
- ID: 90970
Цитировать
Аннотация
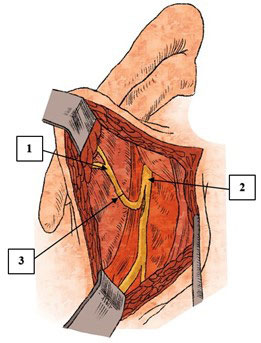
Поражения лицевого нерва являются одним из наиболее часто встречающихся видов патологии периферической нервной системы. В структуре поражений черепных нервов эта патология занимает первое место. Клиническая картина повреждений лицевого нерва различного генеза довольно однообразна и проявляется стойким парезом или параличом мимической мускулатуры. В литературе описано большое количество различных высокоэффективных методик, направленных на восстановление функции лицевого нерва и мимической мускулатуры, примерами которых служат многочисленные консервативные и оперативные способы лечения невропатии лицевого нерва. В обзоре представлен наиболее распространённый способ хирургического лечения паралича мимической мускулатуры — невротизация лицевого нерва. Суть такого оперативного вмешательства заключается в подшивании к поражённому лицевому нерву ствола или порции отдельных волокон интактного нерва-невротизатора, в качестве которого могут выступать подъязычный, жевательный, диафрагмальный, добавочный, языкоглоточный нервы, а также нисходящая ветвь подъязычного нерва и передние ветви С2–С3 шейных нервов. В настоящее время среди нейрохирургов набирают популярность варианты комбинированного использования различных нервов-доноров и аутовставок в связи с более благоприятными результатами восстановления функции лицевого нерва, а также с индивидуальным подходом к каждому пациенту. Основные этапы невротизации лицевого нерва включают выделение и пересечение лицевого нерва, выделение и пересечение ствола или отдельных волокон невротизатора, выполнение шва нерва способом «конец в конец» или «конец в бок». Особого внимания заслуживает наиболее инновационный способ невротизации лицевого нерва — кросс-пластика лицевого нерва, в ходе которой с помощью аутовставок из икроножного нерва или свободного мышечного трансплантата, включающего нежную мышцу и переднюю ветвь запирательного нерва, производят анастомоз между повреждённым и интактным лицевыми нервами. Процесс восстановления функции лицевого нерва и регрессирование характерной симптоматики занимают длительный промежуток времени и требуют проведения специализированного восстановительного лечения.
Ключевые слова
Полный текст
Об авторах
Богдан Валентинович Скалийчук
Военно-медицинская академия им. С.М. Кирова
Автор, ответственный за переписку.
Email: bogdan_skaliitchouk@mail.ru
ORCID iD: 0000-0002-6024-8142
курсант
Россия, г. Санкт-Петербург, РоссияАлексей Иванович Гайворонский
Военно-медицинская академия им. С.М. Кирова; Санкт-Петербургский государственный университет
Email: don-gaivoronsky@ya.ru
ORCID iD: 0000-0003-1886-5486
докт. мед. наук, проф., каф. нейрохирургии
Россия, г. Санкт-Петербург, Россия; г. Санкт-Петербург, РоссияВячеслав Вадимович Виноградов
Военно-медицинская академия им. С.М. Кирова
Email: ulytreack@gmail.com
ORCID iD: 0000-0001-5930-3805
курсант
Россия, г. Санкт-Петербург, РоссияДмитрий Владимирович Свистов
Военно-медицинская академия им. С.М. Кирова
Email: dvsvistov@mail.ru
ORCID iD: 0000-0002-3922-9887
канд. мед. наук, доц., начальник кафедры нейрохирургии
Россия, г. Санкт-Петербург, РоссияСписок литературы
- Секция СтАР «Ассоциация челюстно-лицевых хирургов и хирургов-стоматологов». Клинический протокол медицинской помощи пациентам с нейропатией лицевого нерва. М.; 2014. 39 с.
- Reich SG. Bell's Palsy. Continuum (Minneap Minn). 2017;23(2, Selected Topics in Outpatient Neurology):447–466. doi: 10.1212/CON.0000000000000447.
- Danny J, Revenaugh PC. Facial reanimation: an update on nerve transfers in facial paralysis. Curr Opin Otolaryngol Head Neck Surg. 2019;27:231–236. doi: 10.1097/MOO.0000000000000543.
- Spencer CR, Irving RM. Causes and management of facial nerve palsy. Br J Hosp Med (Lond). 2016;77(12):686–691. doi: 10.12968/hmed.2016.77.12.686.
- Chang YS, Choi JE, Kim SW, Baek SY, Cho YS. Prevalence and associated factors of facial palsy and lifestyle characteristics: Data from the Korean National Health and Nutrition Examination Survey 2010–2012. BMJ Open. 2016;6(11):e012628. doi: 10.1136/bmjopen-2016-012628.
- Цымбалюк Я.В., Цымбалюк В.И., Третяк И.Б., Медведев В.В., Гурьянов В.Г., Гацкий А.А., Петрив Т.И. Сравнительный анализ различных видов невротизации как метода хирургического лечения периферического пареза лицевого нерва. Новости хирургии. 2020;28(3):299–308. doi: 10.18484/2305-0047.2020.3.299.
- Hohman MH, Hadlock TA. Etiology, diagnosis, and management of facial palsy: 2000 patients at a facial nerve center. Laryngoscope. 2014;124:E283–E293. doi: 10.1002/lary.24542.
- Gordin E, Lee TS, Ducic Y, Arnaoutakis D. Facial nerve trauma: evaluation and considerations in management. Craniomaxillofac Trauma Reconstr. 2015;8(1):1–13. doi: 10.1055/s-0034-137252.
- Шургая Ц.М., Неробеев А.И., Караян A.C., Мясковская Е.М. Возможности нейроневротизации при лечении больных с лицевыми параличами. Стоматология. 1995;74(4):33–39.
- Калакуцкий Н.В., Пахомова Н.В., Петропавловская О.Ю. Алгоритм выбора различных методик лечения больных с опухолями околоушной слюнной железы и параличом мимической мускулатуры. Международный журнал прикладных и фундаментальных исследований. 2016;(12-9):1637–1640. EDN: XUVOXX.
- Гребенюк В.И., Чуприна Ю.В. Хирургическое лечение параличей лицевых мышц. Л.: Медицина; 1964. 155 с.
- Зотов А.В., Рзаев Д.А., Дмитриев А.Б., Чернов С.В., Мойсак Г.И. Оценка ближайших результатов хирургического лечения больных с лицевым параличом методом тригеминальной невротизации. Вопросы нейрохирургии. 2016;(4):31–39. doi: 10.17116/neiro201680431-39.
- Злотник Э.И., Склют И.А., Смеянович А.Ф., Короткевия Е.А. Лицевой нерв в хирургии неврином слухового нерва. Минск: Беларусь; 1978. 143 с.
- Каверина В.В. Регенерация нервов при нейропластических операциях. Л.: Медицина; 1975. 215 с.
- Brown S, Isaacson B, Kutz W, Barnett S, Rozen SM. Facial nerve trauma: Clinical evaluation and management strategies. Plast Reconstruct Surg. 2019;143(5):1498–1512. doi: 10.1097/PRS.0000000000005572.
- Говенько Ф.С. Хирургия повреждения периферических нервов. СПб.: Феникс; 2010. 384 с.
- Цимбалюк Я.В., Третяк І.Б., Гацький О.О., Лузан Б.М., Петрів Т.І., Цимбалюк В.І. Диференційовані методи хірургічного лікування хворих з наслідками ушкоджень лицевого нерва. Травма. 2019;20(6):45–52. doi: 10.22141/1608-1706.6.20.2019.186034.
- Matos Cruz AJ. Facial nerve repair. Treasure Island (FL): StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK560623/ (access date: 14.11.2021).
- Sánchez-Ocando M, Gavilán J, Penarrocha J, González-Otero T, Moraleda S, Roda JM, Lassaletta L. Facial nerve repair: the impact of technical variations on the final outcome. Eur Arch Otorhinolaryngol. 2019; 276:3301–3308. doi: 10.1007/s00405-019-05638-8.
- Tarek A. Amer, Mohamed S. El Kholy. The split hypoglossal nerve versus the cross-face nerve graft to supply the free functional muscle transfer for facial reanimation: A comparative study. J Plast Reconstr Aesthet Surg. 2018;71:750–757. doi: 10.1016/j.bjps.2018.01.008.
- Нечаева А.С., Улитин А.Ю., Пустовой С.В., Тастанбеков М.М. Опыт реиннервации лицевого нерва подъязычным нервом для коррекции послеоперационной дисфункции лицевого нерва. Российский нейрохирургический журнал имени профессора А.Л. Поленова. 2019;21(3):32–37. EDN: ZJVHYN.
- Socolovsky M, Roberto S, Masi G. Treatment of complete facial palsy in adults: comparative study between direct hemihypoglossal-facial neurorrhaphy, hemihipoglossal-facial neurorrhaphy with grafts, and masseter to facial nerve transfer. Acta Neurochir. 2016;158;945–957. doi: 10.1007/s00701–016–2767–7.
- Yetiser S. Immediate hypoglossal-facial anastomosis in patients with facial interruption. J Craniofac Surg. 2018;29(3):648–650. doi: 10.1097/SCS.0000000000004150.
- Samii M, Alimohamadi M, Khouzani RK, Rashid MR, Gerganov V. Comparison of direct side-to-end and end-to-end hypoglossal-facial anastomosis for facial nerve repair. World Neurosurg. 2015;84(2):368–375. doi: 10.1016/j.wneu.2015.03.029.
- Venail F, Sabatier P, Mondain M, Segniarbieux F, Leipp C, Uziel A. Outcomes and complications of direct end-to-side facial-hypoglossal nerve anastomosis according to the modified May technique. J Neurosurg. 2009;110(4):786–791. doi: 10.3171/2008.9.JNS08769.
- Dziedzic TA, Kunert P, Marchel A. Hemihypoglossal-facial nerve anastomosis for facial nerve reanimation: Case series and technical note. World Neurosurg. 2018;118:460–467. doi: 10.1016/j.wneu.2018.06.217.
- Gao Z. Neurorrhaphy for facial reanimation with interpositional graft: Outcome in 23 patients and the impact of timing on the outcome. World Neurosurgy. 2019;19:1–16 doi: 10.1016/j.wneu.2019.02.124.
- Biglioli F, Frigerio A, Colombo V, Colletti G, Rabbiosi D, Mortini P, Dalla Toffola E, Lozza A, Brusati R. Masseteric-facial nerve anastomosis for early facial reanimation. Craniomaxillofac Surg. 2012;40(2):149–155. doi: 10.1016/j.jcms.2011.03.005.
- Hontanilla B, Marre D, Cabello A. Masseteric nerve for reanimation of the smile in short-term facial paralysis. Br J Oral Maxillofac Surgery. 2014;52(2);118–123. doi: 10.1016/j.bjoms.2013.09.017.
- Collar RM, Byrne PJ, Boahene KD. The subzygomatic triangle: Rapid, minimally invasive identification of the masseteric nerve for facial reanimation. Plast Reconstr Surg. 2013;132(1):183–188. doi: 10.1097/prs.0b013e318290f6dc.
- Boahene K. Reanimating the paralyzed face. F1000 Prime Rep. 2013;5–49. doi: 10.12703/P5-49.
- Fournier HD, Denis F, Papon X, Hentati N, Mercier P. An anatomical study of the motor distribution of the mandibular nerve for a masseteric-facial anastomosis to restore facial function. Surg Radiol Anat. 1997;19:241–244. doi: 10.1007/BF01627866.
- Гайворонский И.В., Родионов А.А., Гайворонская М.Г., Ничипорук Г.И., Шашков В.А. Роль жевательных мышц и височно-нижнечелюстного сустава в реализации контрфорсной функции нижней челюсти. Вестник Российской военно-медицинской академии. 2017;60(4):158–163. EDN: YLNRTA.
- Albathi M, Oyer S, Ishii LE, Byrne P, Ishii M, Boahene KO. Early nerve grafting for facial paralysis after cerebellopontine angle tumor resection with preserved facial nerve continuity. JAMA Facial Plast Surg. 2016;18(1);54–60. doi: 10.1001/jamafacial.2015.1558.
- Biglioli F, Colombo V, Rabbiosi D, Tarabbia F, Giovanditto F, Lozza A, Cupello S, Mortini P. Masseteric-facial nerve neurorrhaphy: results of a case series. J Neurosurg. 2017;126(1):312–318. doi: 10.3171/2015.12.jns14601.
- Hontanilla B, Marré D. Comparison of hemihypoglossal nerve versus masseteric nerve transpositions in the rehabilitation of short-term facial paralysis using the Facial Clima evaluating system. Plast Reconstr Surg. 2012;130(5):662–672. doi: 10.1097/PRS.0b013e318267d5e8.
- Zhang S, Hembd A, Ching CW, Tolley P, Rozen SM. Early masseter to facial nerve transfer may improve smile excursion in facial paralysis. Plast Reconstr Surg Glob Open. 2018;15;6(11):e2023. doi: 10.1097/GOX.0000000000002023.
- Vila PM, Kallogjeri D, Yaeger LH, Chi JJ. Powering the gracilis for facial reanimation: A systematic review and meta-analysis of outcomes based on donor nerve. JAMA Otolaryngol Head Neck Surg. 2020;146(5):429–436. doi: 10.1001/jamaoto.2020.0065.
- Boahene KO, Owusu J, Ishii L, Ishii M, Desai S, Kim I, Kim L, Byrne P. The multivecto gracilis free functional muscle flap for facial reanimation. JAMA Facial Plast Surgery. 2018;20(4);300–306. doi: 10.1001/jamafacial.2018.0048.
- Viterbo F. Secondary procedures in facial reanimation. In: Grotting JС, editor. Reoperative aesthetic & reconstructive plastic surgery. 2nd ed. St. Louis, Missouri: Qualty Medical Publishing; 2007. р. 859–879.
- Kim MJ, Kim HB, Jeong WS, Choi JW, Kim YK, Oh TS. Comparative study of 2 different innervation techniques in facial reanimation cross-face nerve graft-innervated versus double-innervated free gracilis muscle transfer. Ann Plast Surg. 2020;84(2):188–195. doi: 10.1097/sap.0000000000002034.
- Park Seong Oh, Ha Jeong Hyun, Kim Il‐Kug, Jin Ung Sik, Chang Hak. Single‐stage cross‐facial nerve grafting has a result equivalent to that of two‐stage cross‐facial nerve grafting. Microsurgery. 2020;40(2):175–182. doi: 10.1002/micr.30448.
Дополнительные файлы