Результаты двухэтапного ортодонтического лечения ребёнка с зубоальвеолярной формой дистальной окклюзии
- Авторы: Аюпова Ф.С.1, Хотко Р.А.1
-
Учреждения:
- Кубанский государственный медицинский университет
- Выпуск: Том 103, № 1 (2022)
- Страницы: 133-142
- Раздел: Клинические наблюдения
- Статья получена: 21.05.2021
- Статья одобрена: 24.11.2021
- Статья опубликована: 07.02.2022
- URL: https://kazanmedjournal.ru/kazanmedj/article/view/70895
- DOI: https://doi.org/10.17816/KMJ2022-133
- ID: 70895
Цитировать
Аннотация
Актуальность. В ходе реабилитации детей с дистальной окклюзией не всегда удаётся достичь желаемого результата. В этой связи важными являются факторы, влияющие на результаты лечения дистальной окклюзии у детей в разных периодах формирования прикуса.
Цель. Изучить результаты двухэтапного ортодонтического лечения у детей с зубоальвеолярной формой дистальной окклюзии на примере клинического случая.
Материал и методы исследования. Анализировали результаты обследования пациента в динамике лечения от 6 до 17 лет. На фотографиях определяли симметричность, пропорциональность отделов лица, эстетичность, тип лица, диагностические модели челюстей. Методом ортопантомографии анализировали состояние временных и постоянных зубов, костной ткани челюстей. Оценивали функциональные нарушения. Ортодонтическое лечение в периоде сменного прикуса проводили при помощи съёмных устройств, в том числе усовершенствованных авторами. В периоде постоянного прикуса применяли брекет-систему с силовыми элементами.
Результаты. Несвоевременное обращение, недостаточный уровень мотивации к выполнению рекомендаций по улучшению осанки и стоматологической помощи способствовали увеличению продолжительности лечения. Сохранение чрезмерного изгиба шейного отдела позвоночника и наклона головы назад, «вредная привычка» давления рукой на подбородок, отказ от миогимнастики затрудняли синхронный рост челюстей. Преждевременная потеря временного моляра с одной стороны привела к асимметрии зубоальвеолярной дуги и нарушению окклюзионных контактов. Для устранения этих деформаций были применены дополнительные ортодонтические устройства. Задержка в зубном ряду временных зубов привела к нарушению сроков прорезывания постоянных зубов и, предположительно, к искривлению их корней. Нарушение формы корней и асимметрия размеров коронок постоянных зубов препятствовали полноценной коррекции их положения с применением высокоэффективной современной несъёмной ортодонтической техники. Аномальное положение зачатков третьих моляров, отказ от своевременного их удаления привели в дальнейшем к усложнению техники операции.
Вывод. На сроки и эффективность ортодонтического лечения пациента с зубоальвеолярной формой дистальной окклюзии оказали влияние нарушение осанки, удаление временного моляра, нарушение сроков прорезывания и асимметрия размеров коронок постоянных зубов, наличие «вредных» привычек и нежелание пациента активно сотрудничать с ортодонтом.
Ключевые слова
Полный текст
Актуальность
Дистальная окклюзия (ДО) — распространённая патология, которую выявляют не менее чем у 11% детей при профилактическом осмотре и более чем у 40% детей, обратившихся за ортодонтическим лечением, в том числе у детей Краснодарского края [1–5].
ДО в периоде постоянного прикуса нередко сочетается с аномалиями формы и размеров зубных дуг, тесным положением зубов, аномалиями положения резцов, вестибулопозицией клыков, что вызывает у пациента эстетический дискомфорт, приводит к ухудшению гигиены полости рта и влияет на качество жизни пациентов [1, 2, 6–9].
Комплексная реабилитация детей с ДО направлена на достижение гармоничности лица, нормализацию положения зубов, формы и размеров зубных рядов и их соотношения, функционального состояния жевательных и мимических мышц [1, 2, 7, 10–13].
Ортодонтическое лечение, начатое при первых признаках формирующейся ДО, сопровождается продолжительным применением съёмных и несъёмных ортодонтических устройств, перестройкой состояния жевательных и мимических мышц, нормализацией функций дыхания, жевания, глотания, речи [1, 2, 6, 9–21].
В ходе реабилитации детей с ДО не всегда удаётся достичь желаемого результата. В этой связи представляют интерес факторы, влияющие на результаты лечения ДО у детей в разных периодах формирования прикуса.
Цель
Изучить результаты двухэтапного ортодонтического лечения у детей с зубоальвеолярной формой ДО на примере клинического случая.
Материал и методы исследования
Проведён подробный анализ материалов, отражающих результаты лечения ребёнка в динамике в возрасте от 6 до 17 лет, в их числе медицинская карта стоматологического больного, фотографии лица, диагностические модели челюстей, ортопантомограммы.
Предварительный диагноз формулировали на основании данных основных (клинических) методов исследования — опрос, осмотр, клинические функциональные пробы. При опросе уточняли вероятные причины возникновения ДО и жалобы пациента и его родителей. При осмотре изучали отклонения конфигурации лица от общепринятых критериев нормы, а также проявления зубочелюстных аномалий. Функциональная проба по Эшлеру–Биттнеру демонстрировала состояние профиля лица при сагиттальных перемещениях нижней челюсти в сравнении с критериями нормальной окклюзии по Энглю.
Для уточнения полученных сведений применяли дополнительные (инструментальные) методы: фотометрию лица, измерение диагностических моделей челюстей, ортопантомографию. На фотографиях лица в прямой проекции изучали симметричность, пропорциональность, определяли тип лица по Izard. В боковой проекции оценивали профиль, эстетичность лица по методу Ricketts. На диагностических моделях челюстей измеряли высоту и ширину коронок постоянных зубов в сравнении с нормой по В.Л. Устименко. Пропорциональность сегментов зубных рядов изучали по методам Tonn, Gerlach. Ширину, длину, симметричность зубных рядов оценивали с применением методов Pont, Korkhaus, Ф.Я. Хорошилкиной [1–3, 6, 20].
Методом ортопантомографии проводили оценку зубоальвеолярных областей, временных и постоянных зубов, костной ткани верхней и нижней челюстей, височно-нижнечелюстных суставов [22–24].
Проведённое исследование соответствует стандартам Хельсинкской декларации (Declaration Helsinki). В медицинской карте ортодонтического пациента (учётная форма №043-1/у), утверждённой приказом Минздрава России от 15.12.2014 №834н, есть информированное согласие на проведение ортодонтического лечения и использование обезличенных фотографий его зубов и полости рта («я разрешаю использовать фотографии моих зубов и полости рта без указания моих имени и фамилии»).
Результаты и обсуждение
Из медицинской карты следует, что за ортодонтической помощью пациент Л. впервые обратился в возрасте 5 лет с жалобами на неправильное положение нижних резцов, которое родители выявили в период их прорезывания.
Из анамнеза. Ребёнок родился в срок, доношенным, рос и развивался в соответствии с возрастом. Соматические заболевания на момент обращения не выявлены. Наследственный характер зубочелюстных аномалий не установлен. К стоматологу за лечением кариеса зубов не обращались, зуб 8.4 удалили по причине осложнённого кариеса в возрасте 6 лет.
Конфигурация лица пациента изменена незначительно. Однако были выявлены чрезмерный изгиб шейного отдела позвоночника и наклон головы назад, что рассматривали как фактор риска формирования нижней микро/ретрогнатии и ухудшения профиля лица [25].
При осмотре полости рта выявлено отсутствие в зубном ряду зуба 8.4, оценённое нами как фактор риска возникновения деформации с укорочением нижнего зубного ряда на стороне удаления [26–28].
Взаимоположение дистальных поверхностей коронок верхних и нижних вторых временных моляров в одной плоскости предполагало прорезывание первых постоянных моляров по II классу Энгля.
По результатам обследования был сформулирован диагноз: «Нейтральная окклюзия, сужение зубных рядов, тесное положение резцов. Вторичная адентия зуба 8.4».
Пациенту была рекомендована лечебная физкультура для нормализации осанки. Изготовлены съёмные пластиночные устройства, расширяющие зубные ряды. Восстановлен дефект нижнего зубного ряда справа для предупреждения нежелательной миграции зубов в сторону дефекта, сокращения бокового сегмента и нарушения контактов зубов-антагонистов.
Предложенные меры были предназначены для устранения имеющихся отклонений от нормы, профилактики отрицательного воздействия выявленных факторов риска и создания условий для формирования физиологической окклюзии. Однако пациент отказался пользоваться ортодонтическими устройствами и не посещал ортодонта в течение 1,5 лет.
В возрасте 8 лет пациент повторно обратился к ортодонту с жалобами на тесное положение нижних резцов. Сохранялись чрезмерный изгиб шейного отдела позвоночника и наклон головы назад. Уменьшение высоты нижней трети лица в сравнении с высотой средней трети лица на 2,0 мм сопровождалось незначительными изменениями конфигурации лица.
Лицевой морфологический индекс по Izar оказался равным 87,5%, что не противоречило сведениям о нарушении пропорциональности среднего и нижнего отделов лица и уменьшении высоты нижнего отдела лица (oph-sn) >(sn-gn). Пропорциональность отделов нижней трети лица была также нарушена (sn-st):(st-gn)=1:2,2.
На фотографиях лица в боковой проекции контуры губ и мягких тканей подбородка оставались в профильном поле Дрейфуса. Профиль лица выпуклый (угол n-sn-pg=164°). Выступающие точки губ не касались эстетической линии по Ricketts (pn-pg).
При осмотре полости рта выявили тесное положение нижних резцов, вторичную адентию зуба 8.4, укорочение правого бокового сегмента и асимметрию нижнего зубного ряда. Диастема между зубами 1.1 и 2.1 сочеталась с недостатком места в зубном ряду для прорезывания боковых резцов верхней челюсти. Средние линии зубных рядов не совпадали. Соотношение зубных рядов в области первых постоянных моляров справа и слева было по II классу, а в области временных клыков слева физиологическое, справа бугорковое, что, по нашему мнению, было следствием смещения зуба 8.3 в сторону дефекта нижнего зубного ряда.
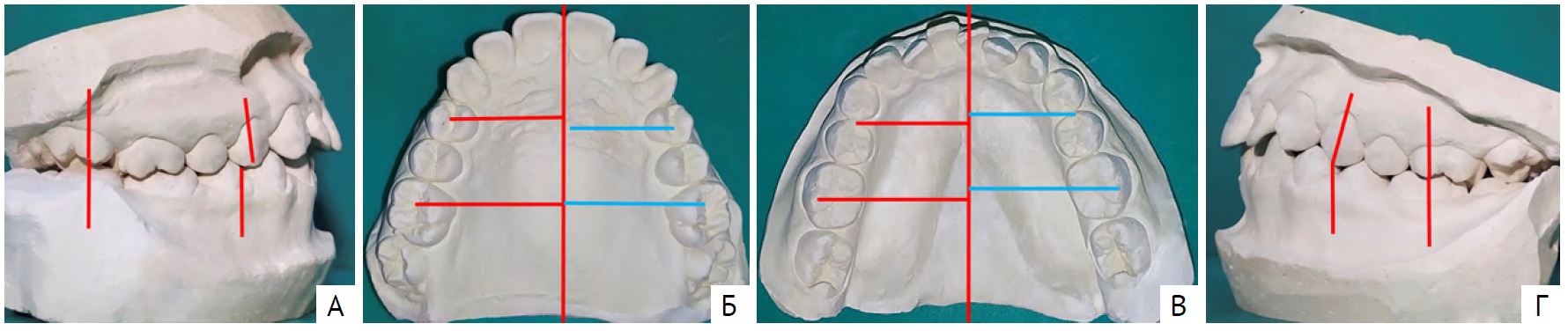
На диагностических моделях челюстей (рис. 1) изучали ширину и длину передних отделов зубных рядов по методам Pont и Korkhaus. По причине отсутствия в ряду зубов 1.2 и 2.2 сумму ширины коронок резцов верхней челюсти вычисляли по формуле с применением индекса Tonn (SI'=si×4/3). Выявили сужение зубных рядов, укорочение правого бокового сегмента и асимметрию нижнего зубного ряда.
Рис. 1. Диагностические модели челюстей пациента Л., возраст 8 лет 6 мес: А — вид справа; Б — модель верхней челюсти; В — модель нижней челюсти; Г — вид слева
На ортопантомограмме направление прорезывания зачатков постоянных зубов было нарушено, выявлен недостаток места в дуге для прорезывания боковых резцов (рис. 2).
Рис. 2. Ортопантомограмма пациента Л., возраст 8 лет 6 мес
Сформулировали диагноз: «ДО, зубоальвеолярная форма. Сужение зубных рядов. Асимметрия нижнего зубного ряда, укорочение бокового сегмента справа. Скученность и тортопозиция нижних резцов. Диастема в области зубов 1.1 и 2.1».
Сравнение формулировки диагноза с предыдущим указывало на ухудшение клинической ситуации, о чём пациент Л. и его родители были предупреждены. Обратили их внимание на наличие факторов риска формирования зубочелюстных аномалий: задержку прорезывания постоянных резцов, асимметрию нижнего зубного ряда, укорочение правого сегмента нижнего зубного ряда.
Составили план лечения: «Расширить зубные ряды при помощи съёмных пластиночных устройств механического действия, удлинить нижний зубной ряд справа. Осуществлять коррекцию направления прорезывания резцов и их положения в зубном ряду, контролировать соотношение первых постоянных моляров и временных клыков. Исключить функциональные нарушения и «вредные привычки».
Отсутствие нарушений гармоничности лица и имеющийся в этом возрасте потенциал роста пациента позволяли прогнозировать положительный результат лечения.
В возрасте 12 лет по причине задержки прорезывания постоянных зубов и неравномерной резорбции корней временных моляров [28] пациент был направлен на ортопантомографию и удаление временных зубов (рис. 3).
Рис. 3. Ортопантомограмма пациента Л. 12 лет
Составлен план лечения: «Расширить зубные ряды при помощи съёмных ортодонтических устройств с винтами и дистализировать первые постоянные моляры до их соотношения по I классу Энгля. Осуществлять контроль прорезывания клыков и премоляров. Исключить функциональные нарушения». Получен удовлетворительный результат лечения (рис. 4).
Рис. 4. Диагностические модели челюстей пациента Л. 13 лет: А — вид справа; Б — модель верхней челюсти; В — модель нижней челюсти; Г — вид слева
Достигнута нейтральная окклюзия. Устранено глубокое резцовое перекрытие. Положение резцов улучшилось, сохранялось тесное их положение. Создано место для прорезывания клыков и премоляров. Обращала на себя внимание задержка сроков прорезывания постоянных клыков, вторых премоляров и вторых моляров. Было рекомендовано исключить функциональные нарушения и «вредные привычки», посещать ортодонта 2 раза в год для контроля над формированием постоянного прикуса. Однако пациент не посещал ортодонта.
В возрасте 15 лет пациент вновь обратился к ортодонту с жалобами на тесное положение нижних резцов.
В результате занятий спортом улучшились осанка и наклон головы. Обращали на себя внимание напряжение мимических мышц лица и незначительное ограничение открывания рта. Конфигурация лица в покое была гармоничной, в момент окклюзии высота нижней трети лица была меньше нижней трети лица на 2,0 мм.
Выявили «вредную привычку» опираться рукой на подбородок. Родителям и пациенту разъясняли необходимость соблюдения правильной осанки, исключения «вредных привычек», функциональных нарушений [29]. На диагностических моделях челюстей (рис. 5) определили правильные фиссурно-бугорковые контакты боковых зубов. Перекрытие нижних резцов оказалось больше 1/2 высоты коронок сопровождалось их тесным положением и тортопозицией.
Рис. 5. Диагностические модели челюстей пациента Л. 15 лет: А — вид справа; Б — модель верхней челюсти; В — модель нижней челюсти; Г — вид слева
Измерение на диагностических моделях челюстей ширины и высоты коронок постоянных зубов показало, что параметры одноимённых зубов асимметричны. Ширина коронок отдельных зубов, в частности, зубов 1.7, 1.1, 2.1, 2.3, 2.7, 3.1, 4.1, превышала среднестатистическую норму (табл. 1).
Таблица 1. Ширина и высота коронок постоянных зубов и их отличия от индивидуальной нормы
Ширина и высота коронок зубов (норма по В.Л. Устименко) | ||||||||||||||
Ширина норма | 8,7–10 | 8,7–10 | 6,0–7,0 | 6,2–7,2 | 7,1–8,1 | 6,0–7,1 | 8,0–9,0 | 8,0–9,0 | 6,0–7,1 | 7,1–8,1 | 6,2–7,2 | 6,0–7,0 | 8,7–10 | 8,7–10 |
Ширина | 12,0 | 9,9 | 6,3 | 6,4 | 7,7 | 7,0 | 8,7 | 8,6 | 6,6 | 7,9 | 6,4 | 6,6 | 9,7 | 10,8 |
Высота норма | 4,5–5,9 | 4,5–5,9 | 5,3–6,9 | 6,6–8,0 | 8,0–9,6 | 7,1–8,5 | 8,2–9,7 | 8,2–9,7 | 7,1–8,5 | 8,0–9,6 | 6,6–8,0 | 5,3–6,9 | 4,5–5,9 | 4,5–5,9 |
Высота | 5,6 | 5,4 | 5,9 | 7,8 | 8,4 | 8,1 | 10,6 | 10,6 | 8,5 | 10,0 | 8,0 | 6,1 | 5,5 | 5,4 |
Зубы в/ч | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
Зубы н/ч | 47 | 46 | 45 | 44 | 43 | 42 | 41 | 31 | 32 | 33 | 34 | 35 | 36 | 37 |
Высота | 5,1 | 5,2 | 6,2 | 7,4 | 8,5 | 8,3 | 9,0 | 8,8 | 8,3 | 8,7 | 7,8 | 6,4 | 6,0 | 5,9 |
Высота норма | 4,5–5,9 | 4,4–6,1 | 6,0–7,3 | 7,2–8,5 | 8,5–10,2 | 7,2–8,7 | 7,0–8,6 | 7,0–8,6 | 7,2–8,7 | 8,5–10,2 | 7,2–8,5 | 6,0–7,3 | 4,4–6,1 | 4,5–5,9 |
Ширина | 10,0 | 10,4 | 7,3 | 7,3 | 6,6 | 5,7 | 5,4 | 5,4 | 5,6 | 6,8 | 7,1 | 7,4 | 11,2 | 10,1 |
Ширина норма | 9,6–10,8 | 10,3–11,7 | 6,5–7,4 | 6,4–7,3 | 6,3–7,2 | 5,6–6,4 | 4,9–5,6 | 4,9–5,6 | 5,6–6,4 | 6,3–7,2 | 6,4–7,3 | 6,5–7,4 | 10,3–11,7 | 9,6–10,8 |
Примечание: в/ч — верхняя челюсть; н/ч — нижняя челюсть.
Отклонения ширины коронок отдельных зубов от среднестатистической нормы способствовали диспропорции сегментов зубных рядов.
Пропорциональность ширины коронок постоянных зубов и протяжённости сегментов зубных рядов по Tonn и Korkhaus представлены в табл. 2.
Таблица. 2. Сегментарный анализ зубных рядов
Сегментарный анализ зубных рядов по методу Gerlach в периоде постоянного прикуса | |||||||||
Lor | Lur | Lol | Lul | SI | si | ||||
сумма | измер. | сумма | измер. | сумма | измер. | сумма | измер. | ||
30,3 | 33,2 | 31,6 | 35,0 | 30,6 | 34,1 | 32,5 | 34,2 | 30,9 | 22,1 |
Примечание: измер. — измерение. Соотношение сегментов зубных рядов следующее: Si/si=1,398; Lor <Lur на 1,3 мм; Lor <Lur на 1,9 мм.
Ортодонтическая помощь в периоде сменного прикуса позволила расширить нижний зубной ряд и устранить его асимметрию, тем самым уменьшить скученность резцов и обеспечить условия для прорезывания клыков и премоляров. В результате многолетней реабилитации деформации зубных рядов у пациента были максимально устранены, однако получить «идеальный» результат не удалось (рис. 6).
Рис. 6. Cегментарный анализ по методу Gerlach зубных рядов верхней (А–Г) и нижней (Д–З) челюстей пациента Л. в возрасте от 8 лет 6 мес до 17 лет
Отклонения ширины коронок зубов от нормы, нарушения пропорциональности сегментов зубных рядов затрудняли формирование окклюзии в соответствии с «шестью ключами» по Эндрюсу.
Кроме того, на ортопантомограмме выявили искривление корней постоянных зубов (рис. 7), что затрудняло их перемещение, а нормализация наклона корней при этом не представлялась возможной.
Рис. 7. Ортопантомограмма пациента Л. 15 лет
Пациент и родители были предупреждены о вероятности возникновения некоторых проблем при перемещении зубов и формировании окклюзии. С планом лечения пациент и его родители согласились. Однако обратились с просьбой удалить зачатки третьих моляров позже, мотивируя семейными обстоятельствами.
В результате ортодонтического лечения брекет-системой Damon Q с соответствующими силовыми элементами получен удовлетворительный результат (рис. 8).
Рис. 8. Диагностические модели челюстей пациента Л. 17 лет: А — вид справа; Б — модель верхней челюсти; В — модель нижней челюсти; Г — вид слева
На ортопантомограмме после завершения ортодонтической коррекции окклюзии выявлены незначительная асимметрия положения зубов и искривление корней отдельных зубов (рис. 9).
Рис. 9. Ортопантомограмма пациента Л. 17 лет
Положение зачатков зубов 2.8, 3.8 и 4.8 в динамике наблюдения от 15 до 17 лет ухудшилось (рис. 10).
Рис. 10. Изменение наклона нижних третьих постоянных моляров пациента Л. относительно окклюзионной плоскости на ортопантомограммах в возрасте 15–17 лет
Это подтверждала динамика наклона осей постоянных зубов и зачатков третьих постоянных моляров относительно окклюзионной плоскости (табл. 3).
Таблица 3. Наклон осей постоянных зубов пациента Л. в динамике наблюдения методом ортопантомографии
Возраст | Наклоны осей в градусах постоянных зубов верхней челюсти | |||||||||||||||
18 | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | |
8,5 лет | 47,4 | 63,1 | 66,6 | 105 | 93 | 85 | 85 | 96 | 101,9 | 93 | 78,8 | 108,9 | 119,2 | 140,9 | ||
12,5 лет | 77,7 | 75 | 90,7 | 91,6 | 90,6 | 77,3 | 93,6 | 93,3 | 108,8 | 86,8 | 92,2 | 98,4 | 110 | 117,8 | ||
15 лет | 65 | 84,9 | 91,2 | 86,7 | 85,5 | 82,8 | 92,2 | 88,5 | 99 | 86,8 | 87,4 | 93,1 | 100,5 | 121,4 | 132,7 | |
17 лет | 70,9 | 71,3 | 82,9 | 85,7 | 86,3 | 81,9 | 87,1 | 87,7 | 101,4 | 91,8 | 87,7 | 97,7 | 97,2 | 113 | 155 | |
Возраст | Наклоны осей в градусах постоянных зубов нижней челюсти | |||||||||||||||
48 | 47 | 46 | 45 | 44 | 43 | 42 | 41 | 31 | 32 | 33 | 34 | 35 | 36 | 37 | 38 | |
8,5 лет | 123,4 | 120,6 | 105,3 | 100,2 | 117,3 | 92 | 91 | 98,7 | 95,8 | 58,2 | 83,7 | 84,8 | 64,3 | 53,5 | ||
12 лет | 115,5 | 111,5 | 103,5 | 93,8 | 96,6 | 91,6 | 91,6 | 93,1 | 98,3 | 89,3 | 81,4 | 81,4 | 66,3 | 62,6 | ||
15 лет | 132,4 | 100,2 | 104,3 | 102 | 96,6 | 94,3 | 89,4 | 87,8 | 85,4 | 92,7 | 83,7 | 85,8 | 78,8 | 74,2 | 81,4 | 130,8 |
17 лет | 141,4 | 112,8 | 111,6 | 113,6 | 97,1 | 104,3 | 83,3 | 90,9 | 85,5 | 86,3 | 77 | 80 | 76,2 | 111,5 | 64,2 | 140,8 |
Таким образом, результаты нашего исследования показали ряд факторов, оказавших влияние на развитие зубочелюстных аномалий и эффективность лечения у пациента с ДО.
Несвоевременное обращение за специализированной стоматологической помощью и преждевременная потеря временного моляра привели к асимметрии нижнего зубного ряда и увеличению тяжести зубочелюстных аномалий.
Недостаточной оказалась мотивация [30] к устранению «вредных привычек». Регулярная опора подбородком на ладонь руки способствовала увеличению степени перекрытия резцов.
Несоблюдение рекомендаций по улучшению осанки и сохранение чрезмерного изгиба шейного отдела позвоночника и наклона головы назад также отразились на формировании окклюзии.
Несвоевременное удаление зачатков третьих постоянных моляров [31] и нарушения развития отдельных постоянных зубов препятствовали полноценной коррекции положения зубов при помощи эффективной современной несъёмной ортодонтической техники (брекет-системы Damon Q).
Выводы
- Конфигурация лица в сагиттальном направлении при зубоальвеолярной форме дистальной окклюзии гармоничная. При сочетании дистальной окклюзии с глубокой резцовой окклюзией возможно уменьшение высоты нижнего отдела лица.
- Преждевременная потеря временного моляра (зуба 8.4), нарушение развития отдельных зубов и задержка их прорезывания, функциональные нарушения и «вредные привычки» способствовали возникновению деформаций нижней зубной дуги, повышению тяжести зубочелюстных аномалий и снижению эффективности вторичной профилактики и ортодонтического лечения пациента с зубоальвеолярной формой дистальной окклюзии.
- Преждевременная потеря временного моляра с одной стороны привела к сокращению протяжённости бокового сегмента и асимметрии зубоальвеолярной дуги, нарушению окклюзионных контактов. Устранение этих деформаций вызвало необходимость применения дополнительных ортодонтических устройств.
- Задержка смены временных зубов предположительно может стать причиной искривления корней прорезывающихся постоянных зубов, является показанием к удалению этих временных зубов.
- Асимметрия размеров коронок зубов и искривление корней отдельных постоянных зубов затрудняли достижение ортодонтического результата в соответствии с общепринятыми «шестью ключами окклюзии» по Эндрюсу.
- На формирование зубочелюстных аномалий и результаты ортодонтического лечения оказали влияние недостаточная мотивация к активному сотрудничеству пациента и его близких со специалистами стоматологического профиля.
- Аномальное направление прорезывания зачатков третьих моляров сохранялось в динамике наблюдения в периоде сформированного постоянного прикуса.
Участие авторов. Ф.С.А. — руководство работой, анализ литературных сведений и результатов исследования; Р.А.Х. — проведение исследования, анализ литературных сведений и результатов исследования.
Источник финансирования. Исследование не имело спонсорской поддержки.
Конфликт интересов. Авторы заявляют об отсутствии конфликта интересов по представленной статье.
Об авторах
Фарида Сагитовна Аюпова
Кубанский государственный медицинский университет
Автор, ответственный за переписку.
Email: farida.sag@mail.ru
ORCID iD: 0000-0002-4194-664X
SPIN-код: 5187-5443
Scopus Author ID: 57193081297
ResearcherId: AAM-4413-2021
канд. мед. наук, доц., каф. детской стоматологии, ортодонтии и челюстно-лицевой хирургии
Россия, г. Краснодар, РоссияРасудан Адамовна Хотко
Кубанский государственный медицинский университет
Email: khotko.rasudana@yandex.ru
ORCID iD: 0000-0003-0711-0838
SPIN-код: 3593-1187
ResearcherId: AAJ-64362021
клин. орд., каф. стоматологии, факультет повышения квалификации и профессиональной переподготовки специалистов
Россия, г. Краснодар, РоссияСписок литературы
- Хорошилкина Ф.Я. Руководство по ортодонтии. 2-е изд., перераб. и доп. М.: Медицина; 1999. 800 с.
- Хорошилкина Ф.Я. Ортодонтия. 2-е изд., испр. и доп. М.: МИА; 2010. 592 с.
- Персин Л.С. Ортодонтия. Национальное руководство. Т. 1. Диагностика зубочелюстных аномалий. Под ред. Л.С. Персина. М.: ГЭОТАР-Медиа; 2020. 304 с. doi: 10.33029/9704-5408-4-1-ONRD-2020-1-304.
- Аюпова Ф.С., Восканян А.Р. Структура зубочелюстных аномалий у детей в регионах России, ближнего и дальнего зарубежья (обзор литературы). Стоматология детского возраста и профилактика. 2016;(3):49–55.
- Аюпова Ф.С., Терещенко Л.Ф. Структура зубочелюстных аномалий у детей, обратившихся за ортодонтической помощью. Курский научно-практический вестник «Человек и его здоровье». 2013;(4):50–54.
- Образцов Ю.Л., Ларионов С.Н. Пропедевтическая ортодонтия. СПб.: СпецЛит; 2007. 210 с.
- Митчелл Л. Основы ортодонтии. Пер. с англ. Под ред. Ю.М. Малыгина. М.: ГЭОТАР-Медиа; 2017. 336 с.
- Espeland LV, Stenvik A. Perception of personal dental appearance in young adults: relationship between occlusion, awareness, and satisfaction. Am J Orthod Dentofacial Orthop. 2008;100(3):234–241. doi: 10.1016/0889-5406(91)70060-A.
- Проффит У.Р. Современная ортодонтия. 5-е издание. М.: МЕДпресс-информ; 2019. 712 с.
- Персин Л.С. Ортодонтия. Национальное руководство. Т. 2. Лечение зубочелюстных аномалий. Под ред. Л.С. Персина. М.: ГЭОТАР-Медиа; 2020. 376 с. doi: 10.33029/9704-5409-1-2-ONRD-2020-1-376.
- Персин Л.С., Шаров М.Н. Стоматология. Нейростоматология. Дисфункции зубочелюстной системы. М.: ГЭОТАР-Медиа; 2013. 360 с.
- Аюпова Ф.С., Хотко Р.А. Современные тенденции выбора тактики и способа лечения растущих пациентов с дистальной окклюзией (обзор литературы). Стоматология детского возраста и профилактика. 2020;20(2):156–159. doi: 10.33925/1683-3031-2020-20-2-156-159.
- Малыгин Ю.М., Пылева Н.В. Оценка эффективности различной ортодонтической аппаратуры при дистальном перемещении боковых зубов. Клиническая стоматология. 2009;(3):64–67.
- Картон Е.А. Организация и планирование комплексной реабилитации пациентов с сагиттальными аномалиями окклюзии. Социальные аспекты здоровья населения. 2015;(3):8.
- Веретенникова О.П., Гвоздева Л.М. Комплексный подход в лечении дистальной окклюзии у детей в период раннего сменного прикуса. Dental Forum. 2014;(4):38–42.
- Дорошенко С.И., Кульгинский Е.А., Стороженко К.В. Особенности ортодонтического лечения пациентов с дистальным прикусом в разные возрастные периоды формирования зубочелюстного аппарата. Современная ортодонтия. 2012;(3):5–12.
- Graber TM, Vanarsdall RLJr. Orthodontics. Current principles and techniques. Book. 5th ed. Mosby; 2011. 994 p.
- Patti A, Perrier G. Clinical success in early orthodontic treatment. Quintessence International; 2005. 124 p.
- Malnagren О, Omblus J, Hagg U, Pancherz H. Treatment with an orthopedic appliance system in relation to treatment intensity and growth periods. A study of initial effects. Am J Orthod Dentofac Orthop. 1987;191:143–151. doi: 10.1016/0889-5406(87)90472-0.
- Набатчикова Л.П., Хорошилкина Ф.Я., Чобанян Арман, Чобанян Армине. Различия в размерах коронок временных моляров и их значение для выбора профилактических мероприятий при сагиттальных аномалиях окклюзии зубных рядов. Российский медико-биологический вестник имени академика И.П. Павлова. 2014;(3):132–138.
- Хорошилкина Ф.Я., Френкель Р., Демнер Л.М., Фальк Ф., Малыгин Ю.М. Диагностика и функциональное лечение зубочелюстно-лицевых аномалий. М.: Медицина; 1987. 304 с.
- Васильев А.Ю. Лучевая диагностика в стоматологии. Национальное руководство. Под ред. А.Ю. Васильева, С.К. Тернового. М.: ГЭОТАР-Медиа; 2010. 171 с.
- Морозова Н.В., Васманова Е.В., Ландинова В.Д., Голочалова Н.В., Иванкина Е.О. Возможность рентгенологических исследований в детской терапевтической стоматологии. Стоматология детского возраста и профилактика. 2014;13(3):3–7.
- Аюпова Ф.С., Павлий Ю.С. Возможности ортопантомографии у детей с зубочелюстными аномалиями. Стоматология детского возраста и профилактика. 2016;(1):34–38.
- Зволинская А.М., Мозолюк Е.Ю. Нарушение осанки детей и подростков как фактор развития неправильного прикуса. Современная стоматология. 2018;(1):90.
- Морозова Н.В., Слабковская А.Б. Влияние ранней потери молочных зубов на формирование постоянных зубов. Ортодонтия. 2016;(4):2–7.
- Яхина З.Х., Ширяк Т.Ю., Камальдинова А.Р. Влияние ранней потери зубов на формирование зубочелюстных аномалий. Современные проблемы науки и образования. 2018;(2):57.
- Аюпова Ф.С., Алексеенко С.Н., Зобенко В.Я., Гайворонская Т.В. Резорбция корней многокорневых временных зубов у детей с зубочелюстными аномалиями по данным ортопантомографии. Стоматология детского возраста и профилактика. 2020;20(3):235–241. doi: 10.33925/1683-3031-2020-20-3-235-241.
- Ушницкий И.Д., Алексеева Т.В., Пинелис И.С., Юркевич А.В., Михальченко Д.В., Давыдов И.Е. Этиологические факторы и патогенетические механизмы формирования и развития деформация зубочелюстной системы. Дальневосточный медицинский журнал. 2019;2:94–99. 2019;2:94–99. doi: 10.35177/1994-5191-2019-2-93-98.
- Зинченко К.С., Дудукалова В.С., Хачатрян А.З., Садовникова Т.Г., Волошина О.В. Мотивация и сотрудничество в ортодонтическом лечении: анализ ответов пациентов подросткового возраста и их родителей. Медицина. Социология. Философия. Прикладные исследования. 2020;(3):7–11.
- Арсенина О.И., Шишкин К.М., Шишкин М.К., Попова Н.В. Третьи постоянные моляры. Их влияние на зубоальвеолярные дуги. Российская стоматология. 2016;2(9):33–40. doi: 10.17116/rosstomat20169233-40.
Дополнительные файлы